My lung cancer surgery went well on Tuesday. I came home yesterday and am resting, watching some shows, and reading for the next few days. The pain is manageable but still slightly annoying. It’s hard to wrap my head around the fact that 25% of my lung was removed only two days ago, and here I am posting about it. Oh, the wonders of modern medicine!
I posted the above to social media, from home, two days after my surgery. I was blissfully unaware of what the next two weeks would have in store for me.
The Surgery
The morning of the surgery, I was relieved to wake up on time after having dreams of being late for my lobectomy. I was in a good mood, had no fear or nervousness, and was mentally prepared, as best I could be, for what was ahead of me.
As we drove to the hospital for our 5:30 am scheduled arrival, I had a few thoughts about not waking up after the surgery and about waking up during surgery. Both were fleeting and did not scare me enough to call up the butterflies.
I had accepted my fate and all that it could bring with it. My only path was forward, and I would not entertain any other thought.
Nearly as soon as I checked in, they took me back to the pre-op area. I undressed, sat on the bed, and then the preparation began. IVs were started, blood was drawn, and I had a quick pre-surgery chat with my surgeon (Dr. B.), and met my anesthesiologist. Then I was presented with a “pain block” procedure that injected pain medicine into the area near my spine. Similar, yet different from the epidural that I had for my son’s c-section.
After all the preparations were complete, the nurse brought Rich and Dawson into the preoperative area, and we began our journey to where the main event would take place. When they traveled as far as was allowed, Rich and Dawson said their goodbyes to me, as I continued on to the OR.
Once in the place where my surgery would soon commence, I assisted in my own transfer from the bed to the operating table. Before I knew it, there was a mask over my face and nose, and I could hear Dr. B. and the anesthesiologist conferring to my left.
Post-Surgery
And boom, my following thoughts were drug-induced and are now buried somewhere in my brain. I remember Rich being there, me feeling high as a kite (which felt so good), and my bed being wheeled to the ICU. I remember feeling happy, relieved, and of course, high.
After they got me all settled in the ICU (I cannot remember all the things they did), Rich and Dawson came in to see me. I remember feeling really good and being amazed at the lack of pain. Now, don’t get me wrong, there was pain, but it was not what I imagined it would be. And, of course, I was still on the pain block (which lasts 12 hours), Tylenol, oxycodone, and Dilaudid, all at the same time.
I knew ahead of time that I would have several incisions, with one of them being 3-4 inches wide, and a chest tube. Even though the drugs dulled the pain considerably, I felt pain and discomfort on my right side and made an effort not to move too much.
The nurse, Miriam (a fantastic human being), gave me the rundown on how the rest of the day would play out:
The Foley catheter would come out soon, yeah!
I was to use the breathing thingy (incentive spirometer) to help expand my lungs. 10 times per hour. I told her I was an overachiever, so she set a higher goal for me.
She wanted to get me up to walk later in the day, and I agreed to meet that goal.
As soon as the doctor liked my progress, the chest tube would be removed, and I would get to go home.
Miriam laid out goals, and as a goal-loving person, I accepted them. And, as a very competitive person, I wanted to rock my recovery and take the nonexistent prize for winning.
There was no way I wasn’t leaving in 24 hours!
Breathing deeply hurt, but I knew I needed to “hit my numbers” with the breathing thingy to be able to go home the next day, so I did hit that thing hard.
Dr. B came by later to see how I was doing and give me an update on the surgery.
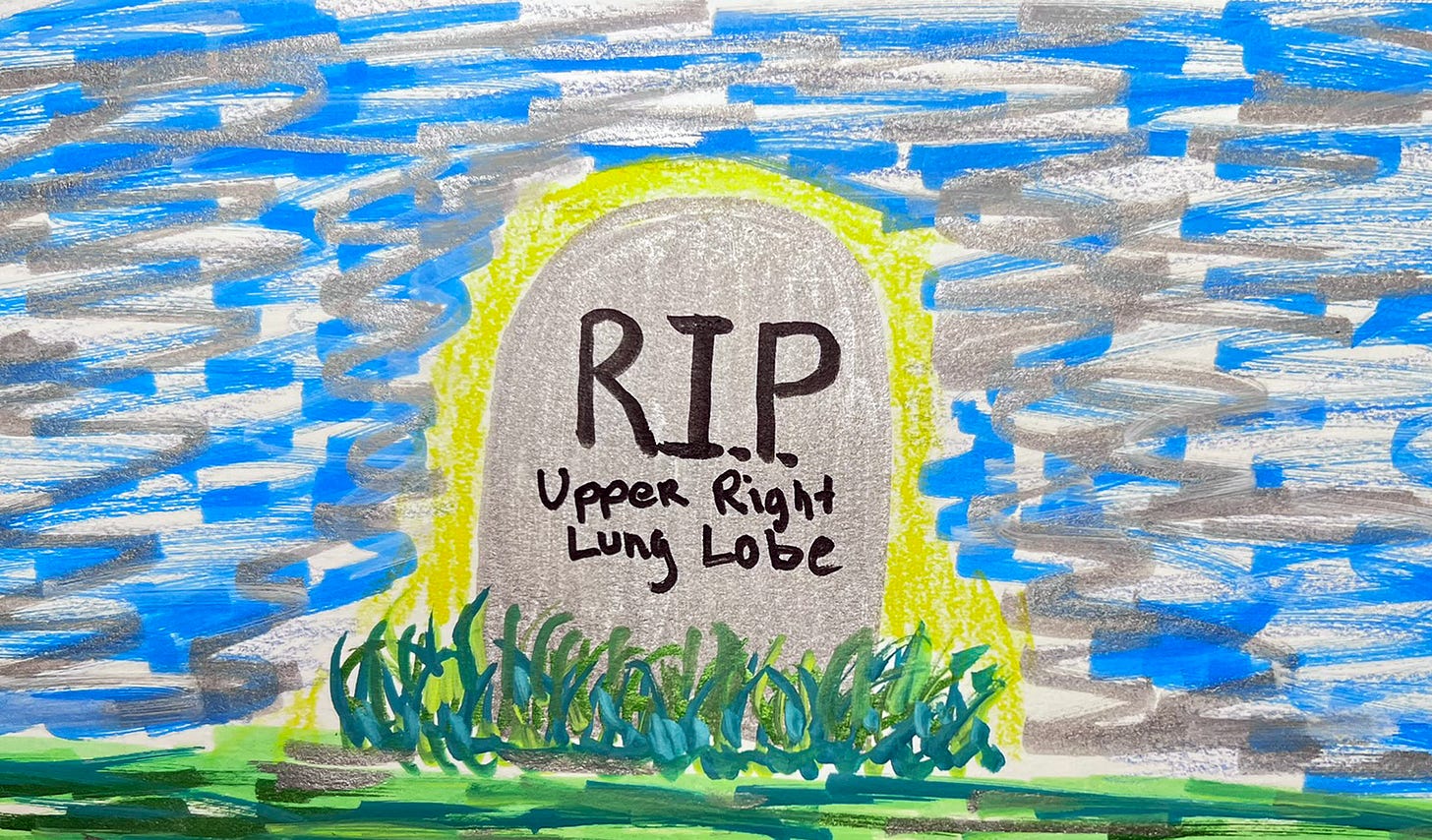
He removed the tumor and its home, the upper lobe of my right lung
10 lymph nodes were also removed
All were sent ot pathology to confirm either localization or the spread of cancer
And here is the most bestest part ever—Dr. B. said my lungs were pink and beautiful, like a baby’s lungs. Which means they healed completely after smoking for 30 years.
Damn, I am a very lucky person.
Well, I did get all this news because I had a cancerous mass in my lung and had to sacrifice 25% of said lung, but I still feel lucky!
Shortly after Dr. B. left, the Foley catheter was removed, and I was setting my sights on walking later in the day. I was nicely medicated for pain and decided to wait until my next dose of Dilaudid to try the walk. Rich and Dawson joined me on my jaunt through the ICU, and when I returned to my bed, I felt victorious. I was sure I would be released the next day.
Because I still had the chest tube inserted, I was not allowed any food or liquid, except for sporadic sips of water. I desperately wanted some Jello, but had to wait until the next day.
I didn’t sleep well that night, but my vitals were stellar, and eventually I enjoyed a few hours of blissful rest. I eagerly awaited the doctor’s rounds, hoping to get confirmation that I would be leaving the hospital later in the day.
Dr. B. came by and said I was his “rockstar patient” and that I would be going home later that day. Less than an hour later, my chest tube was pulled, which was an interesting sensation. It wasn’t painful, but it wasn't pleasant either. The best part was the Jello and apple juice that arrived shortly afterward. It felt good to eat something again.
I wanted to walk more before my discharge later that day, and I did so. I had the option to walk out of the hospital or be wheeled out. I chose the latter because I was unsure how much stamina I would have.
Home to Recovery
Arriving home was terrific, and I was excited to start my 3 weeks of recovery before returning to work. I was determined to “win” the recovery and had high hopes.
The first few nights, I slept on the couch in a sitting position. It wasn’t comfortable, but it wasn’t excruciating either. Unfortunately, I didn’t get much sleep.
When the chest tube was removed, they had to put an enormous amount of tape over it and most of my side to protect the incision until it began to heal. I was not to remove the tape for 72 hours. The tape was painful and limited my range of motion. I told myself that when the tape came off, I would feel much better.
I came home with a few Oxy pills, but they were adamant at the hospital that I should rely on the Tylenol and not the Oxy. I am guessing they tell everyone that to help prevent Oxy abuse. I have a high tolerance to pain, but there were times I really wanted the Oxy, but abided by their directions.
The day the tape came off was spectacular. I was able to put on a bra, which I did not think I would be able to do for weeks. That seemed to help the pain and allowed me to go outside and walk, which I did a couple of times per day. My breathing was good, as was my O2 saturation.
For the next three days, I felt fairly good and was able to sleep in bed instead of on the couch. I felt so good, I did the following:
I made dinner
I made chicken salad
I did laundry
I walked the dog by myself
I held Bodi (my dog) in my left arm and flowers in my right at the same time
I used my right arm to carry and drink from my 32-oz water bottle. When full, it is quite heavy—approximately 3 lbs.
I did some work on my computer
I felt no ill effects from the above tasks at the time. But Wednesday evening, it all came crashing down.
I had a follow-up appointment with Dr. B. that morning, and he said I was healing well and did not need to see me until my 6-month chest CT.
When I went to bed that night, I had an excruciating pain above my right breast. It was sharp, burning, and took my breath away. I could no longer lie down flat.
I headed back to the couch and had to sleep in an upright position. I concluded that all my activities had severely aggravated my pectoral muscle and hindered its ability to heal. The pain was on the same level as my large inquisition just under my armpit, and according to Doctor Google, the incision cut into it. Now this horrifying pain was my constant companion, and I had no idea how long it would last.
I could not lie down flat anymore without pain
The pain would come when I moved my arm a certain way, and the movement that caused the pain would vary
When the pain arrived, it was deep, sharp, burning, and took a few minutes to subside.
I had an appointment with my primary care doctor the next day, and she confirmed the pain was normal, given the surgery. So, I would need to find a way to cope with this new situation. I decided that I needed to be completely immobile for at least three days to hopefully allow my muscles to heal and get me to a more manageable place.
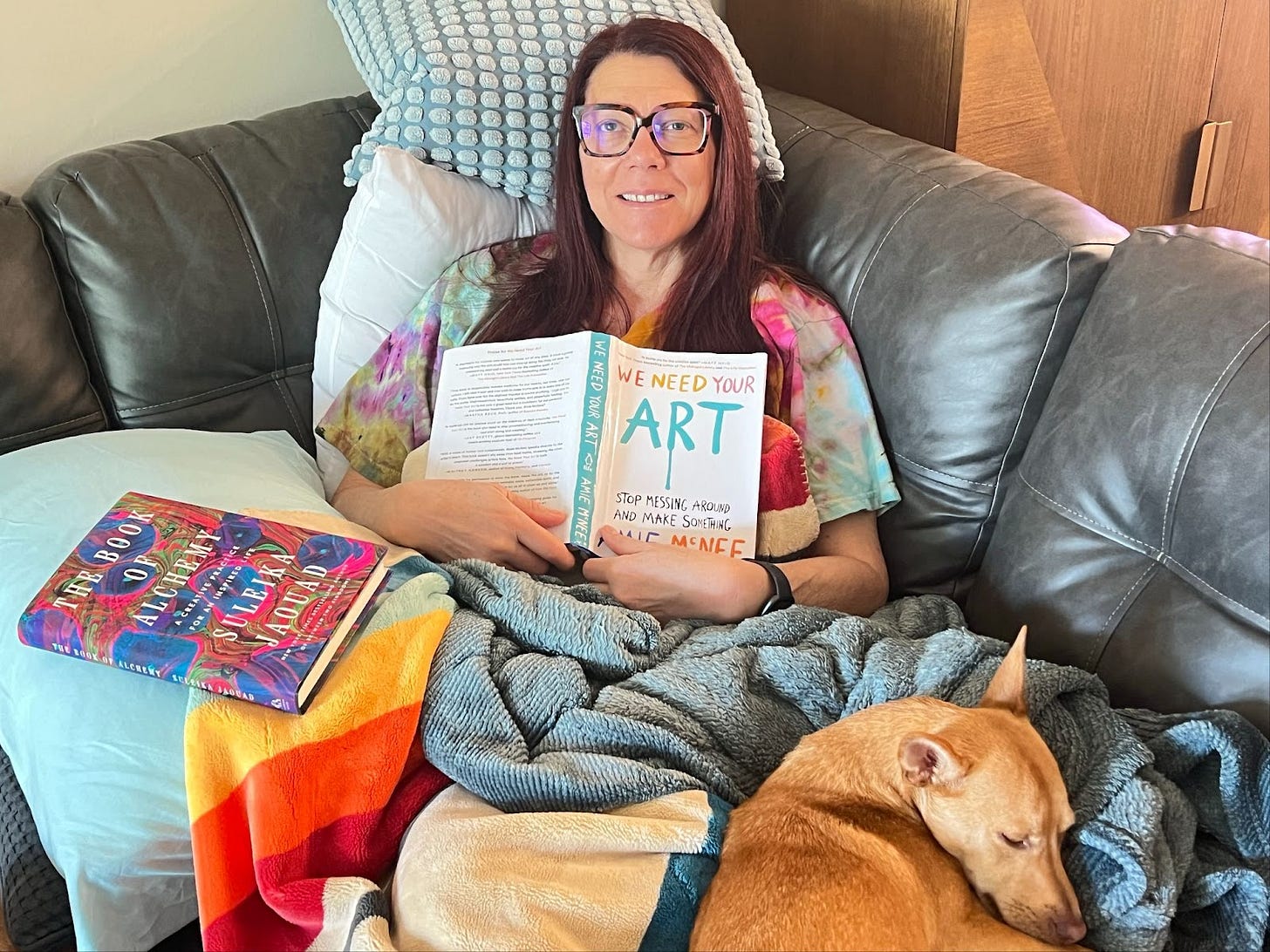
And I was. I did not walk, make any of my own food, fill my water bottle, or anything. I just read and watched TV.
By Sunday, I could shower again, walk outside, and complete a few tasks. But the pain was still strong, and I was still sleeping on the couch in an upright position. My sleep score was low (according to FitBit), as were the hours I slept.
I was in pain. I was tired. And I was mad at myself for causing this.
I was no longer a “rockstar” patient. I was a failure. I failed at my recovery.
Actually, I don’t know for sure if I caused this by my overzealous desire to heal quickly or not. It’s not like I have any experience with healing from an upper lobectomy. And, according to what Doctor Google says (and my doctor, in real life), it’s part of the healing process. My actions may have contributed, or they may not have. I will never know for sure.
But those facts did not stop me from spending way too much time berating myself for causing my recovery failure. However, during that brief trip to the rabbit hole, I realized that I needed to learn how to tame the strong Achiever and Competitor that lived within me if I wanted to heal. Those traits are amazing and necessary in many areas of my life, but I should never use them against myself, which, in this situation, I was doing.
It was a challenging and painful lesson to learn.
Back to the Real World
As I write this, I am exactly three weeks post-op. The pectoral pain is still with me, but it has migrated closer to my side incision, and although strong, it subsides more quickly. I have more range of motion, but still need to be careful how I move and use my right arm. Everything I do is in slow motion compared to my movements pre-surgery. I am being so very careful not to overdo anything and extremely careful not to trigger the pectoral pain, which is still somewhat excruciating.
I still cannot lie flat and had the idea to look for some kind of wedge thingy to help prop me up when I sleep. I found one on Amazon, and it arrived yesterday. My first night with my new “wedgy” friend allowed me to sleep in my own bed and stay mostly asleep through the night, achieving a fairly high sleep score.
My doctors did not adequately express how painful, prolonged, and challenging my recovery would be. I suggested a total of three weeks before I went back to work, and Dr. B. agreed. He did not tell me that I would still have considerable pain, be moving quite slowly, have a swollen abdomen, and a huge amount of numbness. He was pretty clear on the fatigue, though, so there is that.
Even if he had given me more information, I don't think I could have imagined or even adequately prepared for the physical and emotional experience of recovering from a lobectomy. And that’s okay. That’s life. You don’t know until you know.
Throughout this journey, I have chosen to focus on the positives, and I will do the same with my recovery.
My body is free of cancer. The cancer was localized to the tumor, and it has been removed. There was no progression to the lymph nodes (they removed ten).
My breathing has been exceptional since right after the surgery, and I have experienced little shortness of breath
I had the opportunity to binge-watch television shows, read, and do nothing, which is a rare treat.
Rich and Dawson have taken great care of me, and Bodi has not left my side.
Many friends and clients have reached out, sent flowers, gifts, and cards, which warmed my heart immensely.
I was able to attend a magical concert just 18 days after my surgery (Ben Folds playing with the Detroit Symphony Orchestra).
I have had a lot of time to think, which I do a lot anyway, but it seemed different this time.
I'm back to my client work today, although I'm not sure I'll be 100% productive, and that’s okay. Each day, I will feel better and be able to do more.
My intellect, creativity, and work ethic are still intact, and I look forward to getting my brain back into full service. Mentally, I feel good, although this post isn't my best writing. However, you know what? I don’t care. I wrote it, and that is all that matters.
I hope the pain subsides soon so I can get back to painting, but I understand that it may take a few more weeks or longer. And, I am not deluding myself that I will be kayaking any time soon, and that’s okay. I will get back onto the water soon enough.
This was an interesting and challenging journey for me. I feel so very lucky to come out on the other side of cancer so quickly and without complications. My recovery was tougher than I imagined, but in the scheme of things, not as bad as it could have been.
Thank you for following along on my cancer journey!












So proud of you Victoria. 🩷🩷🩷 And happy for all of the love and support circling back to you which you have sent into the world. 🙏😘
I wish my. Mom's Dr. had told her about the swollen belly. That has been her biggest challenge and 6 months out, hers is still a bit swollen. Hopefully yours resolves quicker - you are quite a bit younger that she is 😃😃. So glad to hear that over all things are progressing well and the cancer had not spread beyond that lobe of your lung.